Each year almost 2,400 Australians are diagnosed with bladder cancer, making it one of the top ten cancers. Men are three to four times more likely to be diagnosed with bladder cancer compared to women. The most people diagnosed with bladder cancer are over 60yo but it can occur at any age.
What is bladder cancer?
The bladder is part of he urinary collecting system. It stores urine until an appropriate time occurs when it can be expelled in a process called urination (aka micturition). The bladder lining is composed of cells called urothelial cells. The most common type of bladder cancer (98%) arises from these cells and is called urothelial cancer. These cancers used to be called transitional cell cancers. Other types of bladder cancers are squamous cell (1%) and adenocarcinoma (1%)
Risk factors
There are many recognised risk factors for bladder cancer. These include:
- Smoking – cigarette smokers are up to six times more likely to develop bladder cancer
- Previous cancer treatments –chemotherapy and radiotherapy (to the pelvic area) are associated with an increased risk of bladder cancer. This risk increases 10 years after the initial treatment.
- Older age – most people with bladder cancer are over 60.
- Occupation chemical exposure– chemicals called aromatic amines, benzene products and aniline dyes have been linked to bladder cancer; these chemicals are used in rubber and plastics manufacturing and in the dye industry and sometimes in the work of painters, machinists, printers, hairdressers and truck drivers
- Parasitic bladder infections – bladder cancer is associated with parasitic bladder infestations, particularly schistosomiasis. This blood fluke does not occur in Australian but is endemic to Africa. It presents many years after exposure.
- Long-term catheter use – long-term urinary catheter use may be linked to cancer
- Family history – a small number of bladder cancers are associated with an inherited gene.

Symptoms and signs of bladder cancer
Bladder cancer can is associated with the following presentations:
- Blood in the urine (Haematuria) – the present on blood in the urine, which can be either visible (frank or macroscopic haematuria) or on dip-stick or laboratory testing (microscopic haematuria) should also be investigated further.
- Urinary urgency – the sudden need to pass urine frequently and difficulty in holding in the urine
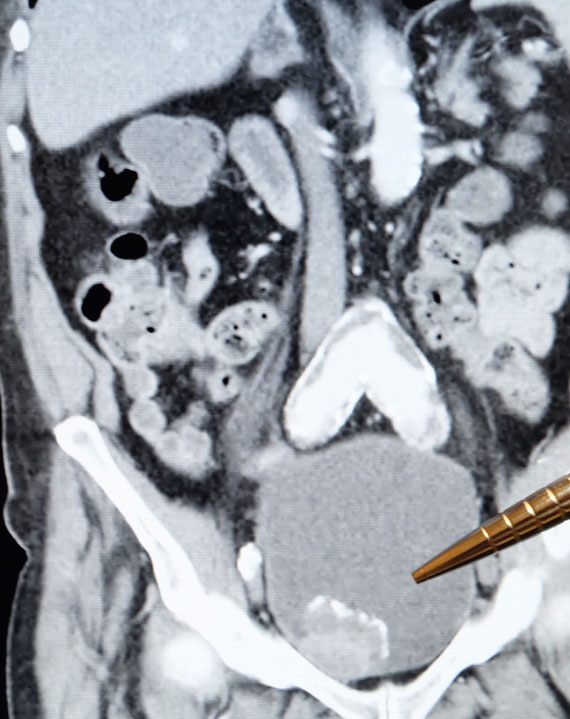
- Lesion in the bladder on imaging – sometimes bladder cancer can be identified incidentally when an ultrasound or CT scan is done for another reason.
- Recurrent urinary tract infections – infections that reoccur frequently or are not eradicated by antibiotics
Diagnosis
To diagnosis bladder cancer, a pathologist needs to see evidence of cancerous changes in a tissue specimen. This means a biopsy is required to make the diagnosis. The biopsy is almost always collected by an endoscopic examination called a cystoscopy. Frequently all of the cancer is also removed at this time.
Treatment
The management of bladder cancer is dependent on the grade and stage of bladder cancer
Grading
Grading answers the question: How aggressive (or fast growing) is my cancer.
Bladder cancer is categorized into low and high grade cancer. Grading is associated with the risk of the cancer growing and spreading as well as the risk of new bladder cancers appearing.
Staging
Staging answers the question: Where is the cancer? Has it spread?
Bladder cancer starts on the surface (lining) of the bladder. It can then grow down through the layers of the bladder.
The layers of the bladder are: Urothelial, lamina propria and muscularis propria (bladder muscle). If the tumour only involves the first two layers it is referred to as a non-muscle invasive bladder cancer. If it also involves the third layer (muscularis propria), it is called referred to as muscle invasive bladder cancer.
The cancer can spread to areas outside the bladder (metastasise). Rarely, spread of cancer outside the bladder has occurred without evidence of muscle invasive.
The location of the tumour is described using a common cancer classification system called TNM: T (tumour), N (Lymph nodes); M (Metastasis). Staging is determined by biopsy of the tumour and imaging (CT scan, Bone scan). These test are best at detecting macroscopic deposits of disease so even if the tests are negative there is still a risk microscopic areas of cancer may be present. This is why even after treatment you need monitoring.
Bladder cancer TNM classification
| TNM | Classification | Features |
| T | a | Papillary tumour confined to the urothelium |
| cis | Flat ‘carcinoma in situ’ confined to the urothelium | |
| 1 | Tumour invades into lamina propria | |
| 2 | Tumour extends into the muscle layer of the bladder | |
| 3 | Tumour extending through bladder and into surrounding fat | |
| 4 | Tumour extending into adjacent structures (prostate, uterus etc) | |
| N | 1 | Single regional lymph node involved |
| 2 | Multiple regional lymph nodes involved | |
| 3 | Distant lymph nodes involved | |
| M | 1 | Distant lymph nodes, bone or other organs involved |
Treatment options
Treatment options for prostate cancer include surveillance, surgery, radiotherapy and pharmaceutical. There are different indications for all three:
| Treatment option | Suitable cancers | Involves |
| Surveillance | Low grade non-muscle invasive cancer | Accepts the factor that while the original cancer has been removed, a ‘field effect’ has occurred, which places you at intermediate risk of a new cancer growing. Involves regular inspection of the bladder to identify and/ or remove cancers while they are still small and easily treated |
| Intra-vesical treatment | High grade non-muscle invasive cancer | Accepts the factor that while the original cancer has been removed, a ‘field effect’ has occurred, which places you at high risk of a new cancer growing. Involves regular instillation of either chemotherapy or immunotherapy (BCG) which prevents cancer recurrence. In addition he bladder is inspected on a regular basis. |
| Radical cystectomy | Muscle invasive but organ confined disease | When cancer is invading the muscle but is still confined to the bladder. Involves surgical removal of the whole bladder. In order to drain urine either a ‘conduit’ or ‘neo-bladder’ is fashioned from small bowel |
| Radical radiotherapy | Muscle invasive but organ confined disease | When cancer is invading the muscle but is still confined to the bladder. Involves irradiating the bladder. |
| Chemotherapy | Muscle invasive but organ confined | Used in combination with either surgery or radiotherapy to increase the likelihood of cure. |
| Chemotherapy or targeted therapy | Metastatic disease | Use to treat cancer outside the bladder. |
KEY POINTS
- Bladder cancer is one of the top ten cancers.
- Common symptoms are blood in the urine, recurrent urinary infections and urinary urgency and frequency.
- Cystoscopy is required to diagnose bladder cancer.
- Bladder cancer is associated with a ‘field effect’ that results in a high risk of new cancers developing even when the original cancer is treated, mandating regular follow-up.
- Once bladder cancer has invade the muscle treatment needs to be much more aggressive for cure to be achieved.
